
FC Lazarus
Me and the Lazarus boys pictured with Kammy at the Sportsman's Dinner on 6th March 2020 just before the first lockdown. It's pre-cancer but still a cool pic!
I've put this site together to talk about my situation and update on the plan I'm working on to get better. I know some people have been asking or perhaps you've heard something and may have been wondering. Well, if so, I hope this will fill you in and bring you up to speed. There’re loads of tangents I could have gone off in as well as many dramas and side stories that I could recount that happened along the way, but I've tried to keep it simple and then present it in a basic way to not over complicate it. I realise it's a bit wordy but it is a story after all, and I have at least tried to jazz it up a bit with those funky scrolling image galleries in an attempt to at least keep it interesting 😜.
Btw, this is my own code and I'm a bit rusty so do bear with me. It looks like the site reads ok on a smartphone, but it's better viewed on a laptop from what I can see. I've added a description on each image by laying the text on top which doesn't seem to display if viewing on a touch screen device - if so, the photos themselves might not make much sense. It'll be a small bug somewhere and I'll look into that later...
Now me and my family have (to our best extent) got our heads around this, I'd love to hear from you. I was really quiet about it last year when it first started and didn't say much back then. It sounds cliche, but it is a lot to come to terms with and understand when you're first told. To understand what's just been said alongside the potential consequences as well as try to figure out what to do next is a complete head-spin! Now we're in 2022 and it's happening all over again, I'd like to try and be a bit more social this time about what's happening and if me telling my story can help anyone else dealing with something similar, or even if I personally can help in some small way then that would be an added bonus.
Feel free to get in touch. I would genuinely love to hear from you. Please don't be shy to ask any questions at all. I'd be happy to share any detail on this no matter how grim if you want it. I'll be as open as you like - Just let me know.

Me and the Lazarus boys pictured with Kammy at the Sportsman's Dinner on 6th March 2020 just before the first lockdown. It's pre-cancer but still a cool pic!

Me smashing Zwift while in training on 14th April 2021 a couple of months out from WTCS Leeds. This was just a month before my diagnosis so cancer will have been well developed at this point. Just didn't know it yet!

Taken on 10th May 2021 about 2 hours after I had my initial ultra sound scan. Walking on the canal at Rodley with Mia and Doug.

All ready for surgery to remove the... well you know! Taken at SJUH, Leeds on 20th May 2021.

The start of outpatient BEP Chemotherapy at SJUH, Leeds on 7th June 2021.

Public Crocs wearer spotted in the Ambulatory Care Unit at SJUH, Leeds on 7th June 2021.

Hotel entrance at Leeds Cancer Centre. SJUH, Leeds on 8th June 2021.

View of Leeds from my room at the Bexley Hotel, Leeds Cancer Centre, SJUH, Leeds on 8th June 2021.

The first PICC Line in the left arm. The one that got infected and led to sepsis on 1st July 2021. The same day as the Lazarus Burger Night at Danny's.

A lovely Omelette & Mash combo thoroughly enjoyed at SJUH for tea on 6th July 2021 while admitted with sepsis. Having been basically unconscious for the previous 4 days, this little delight greeted me when I woke up. Such a treat.
Testicular cancer to be exact. I'll refrain from going into the detail on that particular body area where the primary tumours were found. I’m sure no one wants to know that bit and you'll likely have heard how these things generally occur. In my case it was no different: Find lump > go to docs > go for a scan > review scan results > referral to Urologist for official diagnosis > pick yourself up off the floor > shed tears > hug wife...
In my case, I first met with my GP on Friday, 7th May 2021 who after a quick examination sat me down and reeled out a sentence that is now engraved in my brain and will stay with me forever:
"Simon, I think you need to prepare yourself for the very realistic possibility that this is something sinister."
Oddly, even given the symptoms I'd had for the previous couple of months, I still wasn’t particularly worried about anything until I heard those words. I always assumed things like the 'C-Word' happened to other people and this would be just an infection that eventually antibiotics would clear up. My GP arranged an appointment really quickly for an ultra sound scan which was to be at Wharfedale General Hospital the following Monday, 10th May 2021.
During that scan, I was naturally keen to understand what the technician could see, and I could tell she was a bit reluctant at that stage to relay too much. She did seem to have a worried look on her face and I kept asking to know what she could see. She just wanted to manage expectation properly which I totally get, I would too. She did eventually confirm she could see three lumps but was unable to confirm what they were. Obviously, that was a worry, but was by no means a diagnosis and I was advised to call my GP the next day for the results. Having made that call to my GP first thing the next morning, he explained that the images had been reviewed by the Consultant Radiologist at Wharfedale General Hospital the previous evening and my case had already been referred as urgent to the Urology department at St James’ University Hospital in Leeds.
It was then that the worrying moved to the next level. Following that call and a long hug with Yvonne, it was then Jimmy (my boss) who got a call later that morning with a very emotional explanation of my situation that he definitely wasn’t expecting.
From the perspective of work - big thanks to Jimmy for listening and understanding. I've no words really, just thanks - you continue to be an immense support as does the business as a whole.
So not to drag this out too much (as I know you’re probably reading this while you should be working and are keen to get back to it), I went to see the Urologist on 17th May 2021 who confirmed I had testicular cancer in the form of 4 tumours which required immediate removal through a surgical procedure called 'Orchidectomy' - (Click the link to read about the joys of that). It was explained that although 4 tumours could be clearly seen from the scan results, only following the removal of those tumours would they be able to confirm for certain if malignant cell growth (active cancer) was present after the Pathologist had completed their examination.
I had surgery three days later on 20th May 2021. It went ok and a week of pain from the groin incision and that hampering me moving around is really all that followed to report on there. I now have a nice 6-inch scar in my abdomen to add to my scar collection of three previous hernia repairs and a one spinal fusion. I was discharged from Urology the next day with appointments planned the following week with Oncology to determine the next steps.
I became an Oncology patient on 2nd June 2021. I learned a lot in the few weeks following the initial diagnosis having known very little previously about cancer and how it worked. It’s the blood tests that reveal all. For example, in a case like mine, blood is taken before surgery and then tested to determine a benchmark level of abnormal white blood cells moving through the stream. The measurement of those abnormal cells are referred to as tumour markers. In a good case, the tumour markers would be expected to drop rapidly following the surgical removal of a primary tumour(s). When that does happen, it becomes a key measure which is used to determine next steps and what further treatment may be needed, if any at all. If it does happen that way and the tumours markers rapidly reduce, then it becomes a good indicator that cancer has not spread to any other part of the body.
In the week after my surgery, I had multiple blood tests and a CT scan followed by my first appointment with the Oncology team. Doing what I do for a job and being well practised at it, I went into that meeting hoping for the best and planning for the worst which I figured to be a sensible approach. Looking back at that strategy now that was a mistake. In hindsight, I should have expected the worst in order to turn anything better into positive. Being the half-full and always optimistic dick that I am, I went in there fully expecting to hear the news that the tumours had all been removed, all the cancer had gone, and all was good in the world again.
Unfortunately that wasn’t to be and the news that followed was a very harsh reality check on how serious this had become. The Oncologist explained that my tumour makers had continued to rise post-surgery and they'd risen even higher again across that whole first week of June, which was confirmed in the latest round of blood tests. The tumour markers had gone so high at that point, they alone were enough to determine the next steps in my treatment even without the results from the CT scan.
So yeah, you’ve guessed it, the cancer had spread. The CT scan would simply highlight where the remaining tumours were in my body, their size and how far the spread actually was. It was explained right there that I would need to go through Chemotherapy in an attempt to control further spread and ultimately kill the cancer.
In hindsight, I should have reflected better on that ominous sentence from my GP one month earlier about being realistic. A stark lesson learned there and a clear action for me to take away and implement better next time.
I began a course of treatment with curative intent on 7th June 2021 which is known as BEP Chemotherapy. BEP is the abbreviation of the 3 drugs used - Bleomycin, Etoposide & Cisplatin (Platinum). My BEP Chemotherapy plan was to be delivered as an out-patient while I stayed in the Bexley Hotel at Leeds Cancer Centre, SJUH, Leeds. The plan was to have 4 cycles of 21 days each which would end on 27th August 2021.
BEP Chemotherapy is not easy and is completely horrible every day. The drugs are highly toxic, and they have an immediate and extreme detrimental effect on how you feel. The side effects are too many to list here and they have varying effects on you. I had my fair share; with the added complication of my PICC Line becoming infected on 1st July 2021. What followed was a 7-night admission to SJUH, Leeds as an in-patient for the treatment of sepsis. That was the worst week of my life to date. Not that I actually remember much of it as I was out of it most of the time - but being so ill and in hospital alone with no family allowed to visit due to Covid restrictions, is not something I will ever take any risk to repeat again.
Sepsis aside and as a basic summary of that time, I would describe the 12 weeks of BEP Chemotherapy and the 6 weeks following rather like waking up every day with the worst hangover you've ever had. I started to feel like myself again in early October 2021.
After BEP Chemotherapy had finished, I had a number of tests and scans in early September to determine the situation and what would need to happen next. The CT scan confirmed that I had several tumours that still remained in my abdomen and although the tumour markers in my blood were back in a normal range and showing no further signs of active cancer, these tumours were considered too big a risk to just leave alone. The likelihood of cancer returning on them was high and they had to be surgically removed.
The procedure I was referred for to remove them is called 'Retroperitoneal Lymph Node Dissection (RPLND). It's a surgical procedure to remove abdominal lymph nodes. I understand it's reasonably common following testicular cancer when Chemotherapy itself may have killed active cancer but yet has failed to melt away all the tumours. Basically, the surgeon opens you up and goes in to mop everything up that is left over - that's kind of how I look at that one. I've added the link above so you can read all about it if you're interested. It will be the greatest scar addition yet to my collection, and a very impressive one at that 😉.
I had a good 6 weeks of recovery from the Chemotherapy once the course had completed and by mid-October I wanted to try and get some day-to-day normality back in life. I met up with Jimmy around that time for a bite to eat to just generally catch up and I was keen to discuss with him the possibility of me returning to work. I'd been off work for 5 months at that point and I'd missed it a lot. It's ok being off work for so long when you're actually unwell and unable, but by that point I was feeling pretty much ok again and I wanted to get back to some form of daily routine again other than lying in bed feeling like crap. Sure, I wasn't 100%, but my hair had grown back and I certainly felt well enough to get back to work and contribute something, even if it was a lighter work load than usual and on a phase back return.
I returned to work on 25th October 2021. It was always on the understanding that I was returning on an interim basis until I had a date confirmed for the RPLND surgery that I was waiting for. Due to Covid, a lot of treatments are on hold or have people waiting on lists due to priorities in the NHS and that's understandable and certainly no different for me. There was no real way of knowing when my surgery would be confirmed. "A few months" was all I'd been told so it was just a case of waiting. It was good to be back at work and catch up with so many people that I'd missed while I'd been off. It was great to feel normal again by having something business related to focus on again in the day ahead, rather than just the plastic bags full of toxic drugs hanging from an IV pole next to me. Which is how most of my day's had been since June.
In the following few weeks and in between working, I continued to have blood tests taken every week by the Oncology team which is just a routine part of post treatment care. It's done so a patient's status can be kept closely monitored and any actions determined if anything needs to change. For me, that change didn't take very long. I'd been back at work 5 weeks when I got the call on 3rd December 2021, to tell me that my tumour markers had again started to rise. After being called back in to hospital for follow up tests later that day, it was soon confirmed that my cancer had come back.
One of those tests was another CT scan which highlighted where in the body the active cancer had resurfaced. It was no real surprise when the results showed several tumours with active cancer in my abdomen. It was the same group of tumours that were already known to be there which were already on plan to be removed. It had always been clearly explained that the risk was very high that cancer could return, it was just unlucky that cancer did return so quickly before the surgery to remove them could happen. With the scan confirmation and the tumour markers from the blood continuing to rise week on week, it was determined that I would need further Chemotherapy. The suggested course of Chemotherapy was going to be different than last time and somewhat more intensive. The concern with my case was thought to be the fact that the might of 4 cycles of BEP Chemotherapy was thrown at it a few months earlier, which was thought to have killed the cancer (as was shown in tests post cycle 4 in early September), but yet it had returned so quickly. So a change to the treatment plan had to be made.
So, to draw the story to a close for now, I started a new treatment plan on 12th January 2022 called TIP Chemotherapy. TIP is the abbreviation of the 3 drugs used - Paclitaxel (Taxol), Ifosfamide & Carboplatin (Platinum). Again, this treatment plan is with curative intent and the odds are still very good that it will work. The plan this time around is to be delivered as an in-patient while admitted to SJUH, Leeds. The treatment will be delivered over 5 cycles and will this time include the addition of stem cell transplants in between cycles. The course is expected to complete around Easter 2022. It's still highly likely that I will need the RPLND surgery once completed, so it's looking like I have no escape from that one, but that will be confirmed for sure once we complete this next treatment phase.
It's strange when I think about cancer now and everything that comes with it. The feeling that over comes you when you're first told you have it, the impact it has on you physically and mentally and the absolute unwavering burden it becomes on all the people in your life who love and care for you. It's beyond hard.
I define my life to date with events like getting my first full time job, buying my first car, leaving home, buying my first house, getting engaged and married and then becoming a dad. Being diagnosed with cancer is a bit like that - it's on the same level. Sure, I know how cheesy it sounds to say it like this, but I don't care - I'll just keep going, taking my medicine, and fighting whatever comes my way in whatever direction this takes me in next. Cancer won't define my life; I'm not going to let it.
Game on.

24th July 2021. Easily one of the best days of the year. So privileged to make this having only been discharged from SJUH that same morning following sepsis and completing BEP Chemo cycle 3. Full on no hair mode at this point. I remember being a bit shaky on my feet that day but managed to make it through to the see the first dance!

Classic moody team pose. Taken at Dave and Janet's wedding on 24th July 2021. You're looking at arguably the 27th highest ranked five-a-side football squad ever to grace the 2001 Pudsey Leisure Centre Wednesday night five-a-side league.

11th September 2021. The end of a lovely meal out with Yvonne, Amy and Mia at Miller & Carter, Horsforth. A couple of weeks after I'd completed BEP Chemo Cycle 4 and was in recovery phase.

Top night out with my mates on 11th December 2021. Making the most of it while I could before being re-admitted for further treatment from January.

Let's not forget the lovely wives! They were out with us that night too on 11th December 2021. Top night - Cheers guys!

Love these guys. It's tough going being away from this lot when I'm in SJUH.

...and let's not forget this little guy. Looking as sharp as ever. 25th December 2021.

Hairy legs is back in SJUH to start TIP Chemo Cycle 1 on 11th January 2021. Don't think these babies will stay hairy for very long though...

A hearty nourishing welcome lunch awaits on re-admission to SJUH on 12th January 2022.

The first TIP Chemo infusion on 12th January 2022. It's called Paclitaxel. It's light sensitive hence the dark bag to cover it. It's heavy going and is delivered alongside the hydration IV at the same time. (Could do with investing in some more curtain hooks though around here?!)
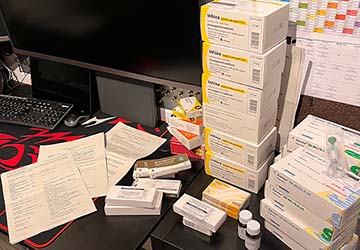
Just a few drugs to take every day in between fusion weeks. Includes 5 x self-administered injections every day! Taken after just arriving home from cycle 1 on 16th January 2022.